Dr Kylie Snook is a Breast Surgeon based in Sydney, and was a guest speaker at our 2023 Annual Scientific Meeting in Auckland, New Zealand. We spoke with her about the treatment changes that have occurred over recent years in breast reconstruction and radiotherapy.
“I’m talking on the conundrum of mixing mastectomy with the need for post-mastectomy radiotherapy breast reconstruction. This is an ever-changing area and something that when I first started practice what I was doing then is very different to what I’m doing now.”
“I’m also exploring my experience over the last 15 years and how my practice changes evolved and where we really need some really great clinical trials that we can use to inform our practice.”
“When we first started doing this, when I started practicing about 15 years ago, the standard treatment for breast cancer, including if someone needed a mastectomy and they needed radiotherapy, a lot of the time surgeons were saying ‘no, we won’t do a reconstruction, let’s not do it because you need radiotherapy and it’ll ruin your reconstruction, we will do it later’.”
“So, women weren’t being given a choice. And so very early on, our practice did a study looking at patient reported outcomes for women who had tissue expander-based reconstruction and then had radiotherapy.”
“Tissue expander reconstruction at that time was a little bit controversial when radiotherapy was needed. But what we’d shown from our study was if you give patients a choice, and they choose a tissue expander, knowing that they may not get the most perfect outcome long term, they were just as happy as the patients who had other types of reconstruction, or had no reconstruction at all.”
“So, I guess what we showed was, if patients are given a choice, that’s the best thing to do. And so, from there our techniques have changed as our practices have evolved and as surgical advances happen. And so, we’ve moved a lot of the time away from two-stage surgeries to just putting the implant straight in.”
“Rather than putting it on the muscle, we put it in front of the muscle and whilst that seems to be a good idea with radiotherapy, I’m certainly seeing negative changes much earlier on than we were doing with the older techniques. So, what I’m looking at is trying to optimize and to improve that for patients long term.”
What is Pectoral Implant Reconstruction?
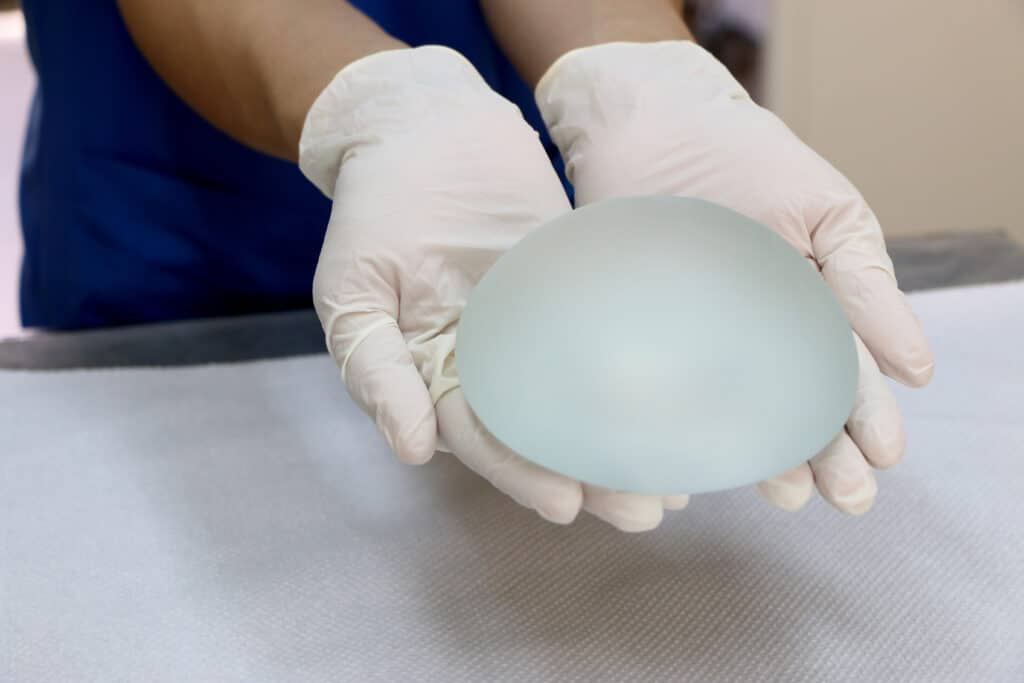
“So, pre-pectoral reconstruction refers to a technique used with breast implant reconstruction as opposed to using our own tissue for reconstruction. So, if we’re using a breast implant, it refers to the position of where we put the implant. So, with pre pectoral, we put the implant in front of the muscle, as opposed to the more traditional method of doing breast reconstruction, which always used to be putting the implant or the tissue expander under the muscle, which is called sub-pectoral.”
“There is some controversial data out there from studies that are quite small. And so there are studies that suggest maybe there’s higher infection rates with pre-pectoral reconstruction. There’s also potentially higher loss of implant from infection because the infections are harder to treat.”
“But then we’ll find another small study which shows that it’s fine. So, the problem with the data out there for us as surgeons is that it is conflicting, and there’s lots of very small studies out there. But what would be ideal is to look at some really good quality randomized studies in this area.”
“Over the last five years, pre-pectoral reconstruction has become a technique that’s used more frequently by breast surgeons because it has been shown to have better cosmetic outcomes. It’s easier, it’s quicker, and it’s associated with less pain during recovery.”
Listen to the Podcast
Dr Kylie Snook is a Breast Surgeon based in Sydney, with an interest in implant reconstruction. We spoke with Dr Snook about the treatment changes that have occurred over recent years in breast reconstruction and radiotherapy.
What is the Radiotherapy Conundrum?
“The radiotherapy conundrum refers to trying to mix in radiotherapy with breast implant reconstruction, because we all know, if you add radiotherapy to an implant-based reconstruction, the outcomes may not be as good as they would be if the patient didn’t have radiotherapy. But there’s much better quality of life outcomes.”
“In terms of complications, we know that it does have potentially worse outcomes than if a patient doesn’t have radiotherapy, but if you need it for your cancer, you have to have it. So, the conundrum is really: how do we mix in an implant-based reconstruction with the radiotherapy and try to get the best outcomes both short and long term?”
“I’d love to see us not giving radiotherapy to patients who have a complete response to chemotherapy, because the current protocols are that if we know a patient’s going to need radiotherapy before chemotherapy, we still give it anyway afterwards, even if the cancer completely goes away.”
“What I would love to see is a clinical trial in these sorts of women who need a mastectomy, looking at if the cancer completely disappears, that we can avoid radiotherapy in the future.”
Support Us
Help us to change lives through breast cancer clinical trials research